Working accuracy of Pulse Oximetry in COVID-19 patients: a clinical evaluation
From the operating rooms, pulse oximetry spread to the recovery room, then the ICUs. Now its use is widespread throughout the hospital. By reducing the incidence of unrecognized hypoxia, pulse oximetry has reduced inpatient mortality immeasurably. Pulse oximeter a valuable tool, but has limitations too.
Doctors Liked to Read More
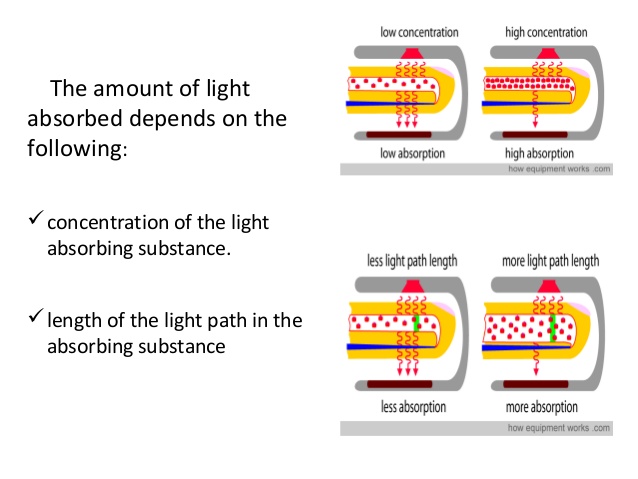
The principle of pulse oximetry
relies on the differences of oxygenated and deoxygenated red cells in
absorption of red and infrared light wavelengths. Oxyhemoglobin and
deoxyhemoglobin absorb these wavelengths in different amounts.
Oximeters have a number of limitations that may lead to inaccurate readings.
With pulse oximetry, a strong, regular pulse is important to obtaining a good signal and accurate reading. Unfortunately, many critically ill patients do not have good pulses anywhere, resulting in inaccurate or fluctuating readings.
The pulse oximeter senses the minute color changes in pulsating blood, and calculates how many oxygen molecules are bound to hemoglobin, or oxygen saturation.
Skin pigmentation
The common fingertip devices that measure oxygen in the blood can sometimes give misleading readings in people with dark skin, according to a report in The New England Journal of Medicine. Skin pigmentation can affect the accuracy of pulse oximetry. In critically ill patients, bias plus precision was greater in black patients, 3.3 + 2.7%, than in white patients, 2.2 + 1.8%; also, a bias greater than 4% occurred more frequently in black patients (27%) than in the white patients (11%).
Carboxyhemoglobin and Methemoglobin levels
Pulse oximeters measure Sao2, which is physiologically related to arterial oxygen tension (Pao2) according to the O2 dissociation curve. Because the dissociation curve has a sigmoid shape, oximetry is relatively insensitive in detecting hypoxemia in patients with high baseline levels of Pao2.
Pulse oximeters use only two wavelengths of light; accordingly, they can discriminiate only two substances, oxyhemoglobin and reduced hemoglobin.
Elevated carboxyhemoglobin and methemoglobin levels can therefore cause inaccurate oximetry readings.
Anemia does not appear to affect the accuracy of pulse oximetry.
Dyes
Intravenous dyes such as methylene blue, indocyanine green, and indigo carmine can cause falsely low Spo2 readings, an effect that persists for up to 20 minutes.
Nail polish, if blue, green, or black, causes inaccurate Spo2 readings, although acrylic nails do not interfere with readings. Falsely low and falsely high Spo2 readings occur with fluorescent and xenon arc surgical lamps.
Low-perfusion states
Low-perfusion states, such as low cardiac output, vasoconstriction, and hypothermia, may impair peripheral perfusion, making it difficult for a sensor to distinguish a true signal from background noise. In patients experiencing hypothermia and poor perfusion during cardiac surgery, only 2 of 20 oximeters (Criticare CSI 503, Datex Satlite, Helsinki, Finland) provided measurements within +4% of the CO-oximeter value. Measurements of Spo2 with a Biox 3700 oximeter had an associated bias greater than ±4% in 37% of patients receiving vasoactive therapy.
An underrecognized and worrisome problem with pulse oximetry is that many users have a limited understanding of how the oximeter functions and the implications of the measurements obtained. One survey revealed that 30% of physicians and 93% of nurses thought that the oximeter measured Pao2. Some clinicians did not recognize that Spo2 values in the high 80s represent seriously low values of Pao2. Of special concern was the observation that some doctors and nurses were not especially worried about patients with Spo2 values as low as 80% (equivalent to Pao2 less than 45 mm Hg).
A more recent audit also demonstrated a deficit in knowledge about the limitation of the technique. Although a majority of trained nurses and physicians were able to identify that shock and hypothermia can alter oximetry readings, less than 50% of nurses and physicians were able to identify that motion artifact, arrhythmias, and nail polish can affect the accuracy of pulse oximetry.
More recent research has highlighted that the accuracy of pulse oximetry can be affected by multiple factors including motion, perfusion, and skin pigmentation.
This retrospective analysis includes 90 paired samples (PaO2 and SpO2) from patients with COVID-19 being downgraded from ICU care. They showed a suboptimal correlation in the range between 5.2% and −4.3%.
There exists a suboptimal accuracy of pulse oximetry in certain patient groups, which may be under-appreciated by healthcare workers.
Occult hypoxia should continue to be considered in certain situations, and commercially available pulse oximeters should be re-evaluated.
In a prospective study in ICU patients, Spo2 signals accounted for almost half of a total of 2525 false alarms. In 235 surgical ICU patients, a recent study revealed that false alarms from the pulse oximeter were secondary to low perfusion (21%), cardiac arrhythmias (9%), motion artifacts (8.4%), shivering (1.7%), and extubation (1.7%).
It is essential to understand that a normal oxygen saturation does not rule out respiratory failure. Hemoglobin may remain saturated with oxygen despite hypoventilation causing rising levels of carbon dioxide. The oxygen saturation may not fall below 90% until the patient is already in serious trouble, especially if the patient is on supplemental oxygen.
Respiratory rate, pCO2, and level of consciousness should all be assessed routinely. Do not rely on the oxygen saturation to warn you of impending respiratory failure.
SpO2 should be interpreted with caution. Arterial blood gas assessment of SaO2 may still be clinically indicated.
Patient measurements at home:
|
1.
Make measurements indoors, at rest, and
during quiet breathing |
|
2.
Use the index or middle finger; avoid the
toes or ear lobes |
|
3.
Only accept values associated with a strong
pulse signal |
|
4.
Observe readings for 30–60 s to identify the
most common value |
|
5.
Measure and record values two to three times
per day |
|
6.
Remove nail polish from the finger on which
measurements are made |
|
7.
Warm cold extremities prior to measurement |
https://bmjopenrespres.bmj.com/content/7/1/e000778
https://www.atsjournals.org/doi/10.1513/AnnalsATS.202005-418FR
https://www.sciencedirect.com/topics/nursing-and-health-professions/oximeter
https://acphospitalist.org/archives/2009/12/tech.htm
https://www.practiceupdate.com/content/accuracy-of-pulse-oximetry-in-covid-19-patients-stepping-down-from-intensive-care/111935/62
https://www.npr.org/sections/health-shots/2020/12/16/947226068/dark-skin-can-lead-to-errors-with-pulse-oximeters-used-in-covid-19-treatment




Comments
You must login to write comment