Elevated Dengue fever activity reported at Dhaka & Chattogram: Clinical Manifestation and Diagnosis of Dengue Fever
Dengue
is endemic in Bangladesh with recurrent outbreaks. Health officials in
Bangladesh have reported elevated dengue fever activity in Bangladesh during
2022. Dhaka and Chattogram has become a hotspot for dengue fever (DF).
Why DF rising in August &
September?
•
The risk of
dengue fever transmission in Bangladesh exists nationwide and year-round;
however, the risk is highest during the rainy season, which typically occurs
June-September. This year in September dengue hospitalsation double against
August figure.
•
Dengue totally
depends on weather. Several factors such
as rainfall, temperature, humidity provide appropriate conditions for its
survival, reproduction, breeding, egg hatching and virus transmissibility.
•
The pattern of
rainfall changed over the past few years. The
expert added that the number of dengue cases usually peaked in July and August,
but low rainfall halted the rise in cases and it started going up again due to
intermittent rain in the beginning of September.
How many infected and how many deaths?
•
According to the
Directorate General of Health Services (DGHS), a total of 14,362 people were
admitted to hospitals since January this year. A total of 8,181 dengue patients
were hospitalised in 26 days of September across the country, which was 57 per
cent of the total hospitalisation this year since January.
•
A total of 11,071
or over 77 per cent of dengue patients were reported to be hospitalised in
Dhaka city and next is Cox’s Bazar.
•
The official
death toll to 53 across the country this year since January, said a press
release of the Directorate General of Health Services. Of the total dengue
deaths this year, 26 people died in Dhaka city, 23 in Chattogram and four in
Barishal division.
•
The data also
showed that 70 per cent of the total deaths occurred between age one and 40
years. Experts believed late
hospitalisation and lack of prompt treatment for the high number of
deaths. Secondary infections are cause for the majority of the
reported deaths up to age 40.
TAKE HOME MESSAGE:
Dengue
is the most common mosquito-borne, viral disease in the world. Dengue virus is
a single stranded positive polarity RNA virus, belongs to the family
Flaviviridae. It is transmitted through the bite of an infected female mosquito
of Aedes species.
There
are 4 distinct, but closely related, serotypes of the virus (DEN-1, DEN-2,
DEN-3 and DEN-4). A fifth addition to the existing serotypes of dengue viruses
is the DENV-5, which was announced in October 2013, after its detection in
Malaysia.
Recovery
from infection by one serotype provides heterotypic or cross-immunity to the
other serotypes. This is only partial and temporary, lasts only a few months,
but homotype immunity is lifelong.
For
this reason, a person can be infected with a dengue virus as many as four times
in his or her lifetime. Subsequent infections (secondary infection) by other
serotypes increase the risk of developing severe dengue.
Stepwise Approach of Dengue Case Evaluation
Step 1 – Overall assessment
1.1
The history should include:
•
Date of onset of fever/illness;
•
Quantity of oral
fluid intake;
•
Diarrhoea;
•
Urine output
(frequency, volume and time of last voiding);
•
Assessment of
warning signs ;
•
Change in mental
state/seizure/dizziness;
•
Other important
relevant history, such as family or neighbourhood dengue, travel to
dengue-endemic areas, co-existing conditions (e.g. infancy, pregnancy, obesity,
diabetes mellitus, hypertension), jungle trekking and swimming in waterfalls (consider
leptospirosis, typhus, malaria), recent unprotected sex or drug abuse (consider
acute HIV-seroconversion illness).
1.2
The physical examination should include
•
Assessment of
mental state;
•
Assessment of
hydration status;
•
Assessment of
haemodynamic status;
•
Checking for
quiet tachypnoea/acidotic breathing/pleural effusion;
•
Checking for
abdominal tenderness/hepatomegaly/ascites;
•
Examination for
rash and bleeding manifestations;
•
Tourniquet test
(repeat if previously negative or if there is no bleeding manifestation).
1.3
The investigation
•
A full blood count (CBC) should be done at the first visit (it may be normal);
Platelet count and haematocrit repeated daily until the critical phase is over.
•
The haematocrit in the early febrile phase could be used as the patient’s own baseline.
•
Decreasing white blood cell and platelet counts make the diagnosis of dengue
very likely.
•
Leukopenia usually precedes the onset of the critical phase and has been associated
with severe disease.
•
A rapid decrease in platelet count, concomitant with a rising haematocrit compared
to the baseline, is suggestive of progress to the plasma leakage/critical phase
of the disease.
•
These changes are usually preceded by leukopenia (≤ 5000 cells/mm3). In the absence
of the patient’s baseline, age-specific population haematocrit levels could be
used as a surrogate during the critical phase.
•
If facilities for a full blood count are not available or if resources are
limited, such as in outbreak settings, a full blood count or microhaematocrit
should be done at the first visit to establish the baseline. This should be
repeated after the 3rd day of illness and in those with warning signs and risk
factors for severe disease.
•
Dengue-specific laboratory tests should be performed to confirm the diagnosis.
However,
it is not necessary for the acute management of patients, except in cases with
unusual manifestations.
Additional
tests should be considered in patients with co-morbidities and severe disease as
indicated. These may include tests of liver function, glucose, serum
electrolytes, urea and albumin.
Step 2 - Diagnosis, Assessment of
disease phase and severity
Diagnosis,
assessment of disease phase and severity on the basis of evaluations of the history,
physical examination and/or full blood count and haematocrit.
Clinicians
should determine whether the disease is dengue, which phase it is in (febrile, critical
or recovery), whether there are warning signs, the hydration and haemodynamic state
of the patient, and whether the patient requires admission. For blood pressure assessment
follow age specific blood pressure chart.
Doctors Liked to Read More
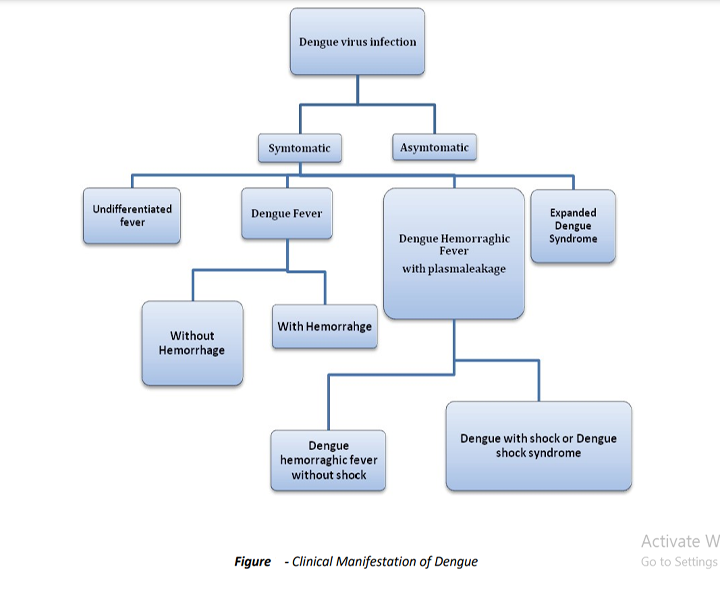
In
most of the cases with dengue virus infection remain asymptomatic; however, it
can cause a wide spectrum of clinical manifestations from mild febrile illness
with spontaneous recovery to hemorrhagic dengue fever (DF) and/or dengue shock
syndrome (DSS).
Dengue
virus infections may be asymptomatic or may lead to undifferentiated fever, dengue
fever, or dengue haemorrhagic fever (DHF) with plasma leakage that may lead to
hypovolaemic shock Dengue Shock Syndrome (DSS).
Many
patients infected with dengue virus remain asymptomatic. Others, after an Incubation
period of 4-7 (range 3-14) days, develop a febrile illness the manifestations of
which are similar and overlapping in nature grouped into ‘Dengue Syndromes’ which encompass the following:
•
Undifferentiated
fever
•
DF
•
DHF
·
DSS
•
Expanded Dengue
Syndrome (rare)
Asymptomatic Infection
The
majority of infections in children under age 15 years are asymptomatic or
minimally symptomatic.
Symptomatic Infection
Undifferentiated
fever
•
Those who have
been infected with dengue virus, especially for the first time (i.e. primary dengue
infection), may develop a simple fever indistinguishable from other viral
infections.
•
Maculopapular
rashes may accompany the fever or may appear during defervescence.
• Upper respiratory and gastrointestinal symptoms are common.
Dengue
fever
Typically,
the onset of DF is sudden with a sharp rise in temperature and is frequently associated
with a flushed face and headache.
Occasionally,
chills accompany the sudden rise in temperature.
The following features are usually
observed:
•
Retro-orbital
pain on eye movement or pressure on eye
•
Photophobia
•
Backache and pain
in the muscles and joints/bones.
•
The other common
symptoms include anorexia and altered taste sensation, constipation, colicky
pain and abdominal tenderness.
It
is noteworthy that these symptoms and signs of DF vary markedly in frequency
and severity.
Fever:
The
body temperature is usually between 39°C and 40°C (102°F to 104°F) and the
fever may be biphasic, lasting 2-7 days in the majority of cases.
Rash:
•
First 2 to 3 days-Diffuse flushing or fleeting eruptions may be seen on the
face, neck and chest
•
Third and fourth day-a conspicuous rash that may be maculopapular or rubella form
•
Afebrile period or defervescence - Petechiae surrounding scattered pale, round areas
of normal skin may appear over the dorsum of the feet, on the legs, and on the
hands and arms. Skin itching maybe observed.
Hemorrhagic manifestations:
In
DF with unusual hemorrhage, Petechiae may be present. Other bleeding such as
massive epistaxis, menorrhagia and gastrointestinal bleeding rarely occur in
DF, complicated with thrombocytopenia. Tourniquet test will be positive in this
case.
Early
laboratory confirmation of clinical diagnosis may be important because some
patients progress within a short period from mild to severe disease and
sometimes to death. Early intervention may be life-saving.
Lab Tests for Diagnosis and Monitoring
The management of DS is based on
clinical judgment rather than laboratory evaluations alone.
Dengue Diagnostic Test
Detection of Antigen: NS1 antigen
(non-structural protein 1):
•
NS1 antigen rapid
test- positive within minutes of starting symptoms.
•
The ELISA NS1
antigen will be positive on first day of illness.
•
This test becomes
negative from day 4-5 of illness.
• Commercial kits for the detection of NS1 antigen are now available in ELISA or rapid test format.
Dengue IgM /IgG test (MAC ELISA or
Rapid ICT):
•
Anti-dengue IgM
specific antibodies can be detected after 5 days of the onset of fever and
highest level achieved after 7 days.
•
It can be
detected in low level up to 1-3 months after fever.
•
In primary dengue
infection- IgM will be more than IgG early period and send IgG at 9 or 10th day
of fever.
•
Level of this IgG
may persist at low levels for decades, indicating past dengue infection.
•
In secondary
dengue infection- higher elevation of anti-dengue specific IgG antibodies and
lower levels of IgM. The higher IgG levels remain for 30–40 days.
• Rapid ICT test provides result within 15 to 20 minutes.
Nucleic Acid Detection:
•
The reverse
transcriptase polymerase chain reaction (RT-PCR)- confirm diagnosis (<5 days
of illness).
•
The amplified DEN
viral RNAs can be detected either by tradition or real time PCR.
• This test is expensive and available only in referral centers.
However, few indirect tests may be
suggestive of DS from the outset. The following tests may be done
1.
Complete Blood Count (CBC):
Including
Total Leucocyte Count, Total Platelet Count and HcT should be done on first consultation
of the patient to have the baseline: Recommendations:
•
All febrile
patients at the first visit within one week
•
All patients with
warning signs.
Leucopenia is common in both adults and children with DF
and has an important diagnostic implication in early period.
The
change in total white cell count (≤5000 cells/mm3) and ratio of neutrophils to
lymphocyte (neutrophils
This
finding precedes thrombocytopenia or rising haematocrit. These changes seen in
DF and DHF.
Thrombocytopenia is observed in some patients with DF. Mild
(100,000 to 150,000 cells/mm3) is common and about half of all DF patients have
platelet count below 100,000 cells/mm3; A sudden drop in platelet count to
below 100,000 occurs before the onset of shock or subsidence of fever. The
level of platelet count is correlated with severity of DHF.
Severe
thrombocytopenia (<100,000/mm3) usually precedes/accompanies overt plasma leakage.
Haematocrit: A slight increase may be due to high fever,
anorexia and vomiting (10%). A sudden rise in haematocrit is observed
simultaneously or shortly after the drop in platelet count.
Haemoconcentration
or rising haematocrit by 20% from the baseline, e.g. from haematocrit of 35% to
≥42% is objective evidence of leakage of plasma.
It should be noted that the level of haematocrit may be affected by early volume replacement and by bleeding.
2.
Biochemical Tests:
Serum AST (SGOT) and ALT (SGPT):
AST
and ALT levels are frequently elevated in both adults and children with DF and
DHF; AST and ALT Levels are significantly higher (5 to 15 times the upper limit
of normal) in patients with DHF. Commonly AST is more than ALT in these cases.
Haematocrit
and Complete blood count if the patient presented within 3 days of fever.
Follow
up testing may be done on 1st afebrile day, but should be done daily once DHF
is suspected.
A
regular haematocrit is more important for management than the thrombocytopenia.
Even
in severe dengue especially with shock) hourly haematocrit is crucial for
management.
Once the platelet count begins to rise
and reaches ≥ 50,000/mm3, daily lab evaluations may be discontinued.
In Special Cases:
•
Hypoproteinemia/Hypoalbuminaemia
(as a consequence of plasma leakage).
•
Hyponatremia is
frequently observed in DHF and is more severe in shock.
•
Hypocalcemia
(corrected for hypoalbuminemia) has been observed in DHF.
•
Metabolic
acidosis is frequently found in cases with prolonged shock.
•
Blood urea
nitrogen is elevated in prolonged shock.
3.
Coagulation Profile:
•
Assays of
coagulation and fibrinolytic factors show reduction in DSS cases.
•
Partial thromboplastin
time and prothrombin time are prolonged in about half and one third of DHF
cases respectively.
•
Thrombin time is
also prolonged in severe cases.
4.
Other tests:
•
Urine R/M/E:
Albuminuria
•
Stool test:
Occult blood is often found in the stool.
•
Chest X-Ray or
Ultrasonography: For detection of pleural effusions or ascites.
•
Other tests for
exclusion: Malaria (MP/ICT), Enteric fever (Blood culture) may be required for
patients with compatible clinical syndromes.
•
Other test as and
when clinically indicated (especially for Dengue expanded syndrome): Serum
Albumin, Liver Function Tests, Renal Function test, Serum electrolytes,
Imaging, ECG, Echocardiography, and CSF etc.




Comments
You must login to write comment